It’ the sixth year that I’ve been working at Bill & Melinda Gates Foundation. One of my expressions in these years is that although Bill Gates' name is well known, most people do not know what Bill & Melinda Gates Foundation does, why it does it, and how it does it. The reason is simple: in the 20 years since its founding, the foundation has been doing something very "unpopular" and "marginal": prevention and control of infectious diseases (AIDS, tuberculosis, malaria, neglected tropical diseases) in low- and middle-income countries, vaccines, drugs and diagnostics. R&D and innovation of tools, poverty reduction and development.
One of the "golden line" running through health and poverty reduction is vaccines, and in 2000, the Foundation made its first donation of $750 million to co-found the Global Alliance for Vaccines (Gavi), a new international organization, and initiated the Coalition for Epidemic Preparedness Innovation (CEPI) to support vaccine development for pandemic diseases.
Because of the new coronavirus epidemic, vaccine development is suddenly in the global spotlight. On the one hand, it seems we should be happy that the work we support is suddenly getting a lot of attention; on the other hand, no one can be happy about the epidemic. In particular, the recent discovery of new cases and reintroduction of control measures in some areas that were once "free" of new coronavirus suggests that society will not be at peace until herd immunity is achieved through a vaccine. Globally, because of the high transmission of the new coronavirus, human society will only be truly safe when everyone in the world is immunized.
So today, I would like to talk about when the New Coronavirus vaccine. When will it be released, and how long will it be before the epidemic can be controlled.
When will the new coronavirus vaccine released?
It could take up to 18 months. But that's actually very fast.
The chain of developing a vaccine is long, often taking 8 to 17 years from preclinical studies to final launch. Even the previous mumps vaccine, which took the shortest time to develop, nearly five years to go from obtaining virus samples to obtaining marketing status.
Compared to traditional vaccines, the development of the new mumps vaccine was "fast". After just a few months of research, four vaccines worldwide are now in Phase II, three are in both Phase I and Phase II, and two are in Phase I trials. Among these 9 vaccines, 5 were developed by Chinese manufacturers.
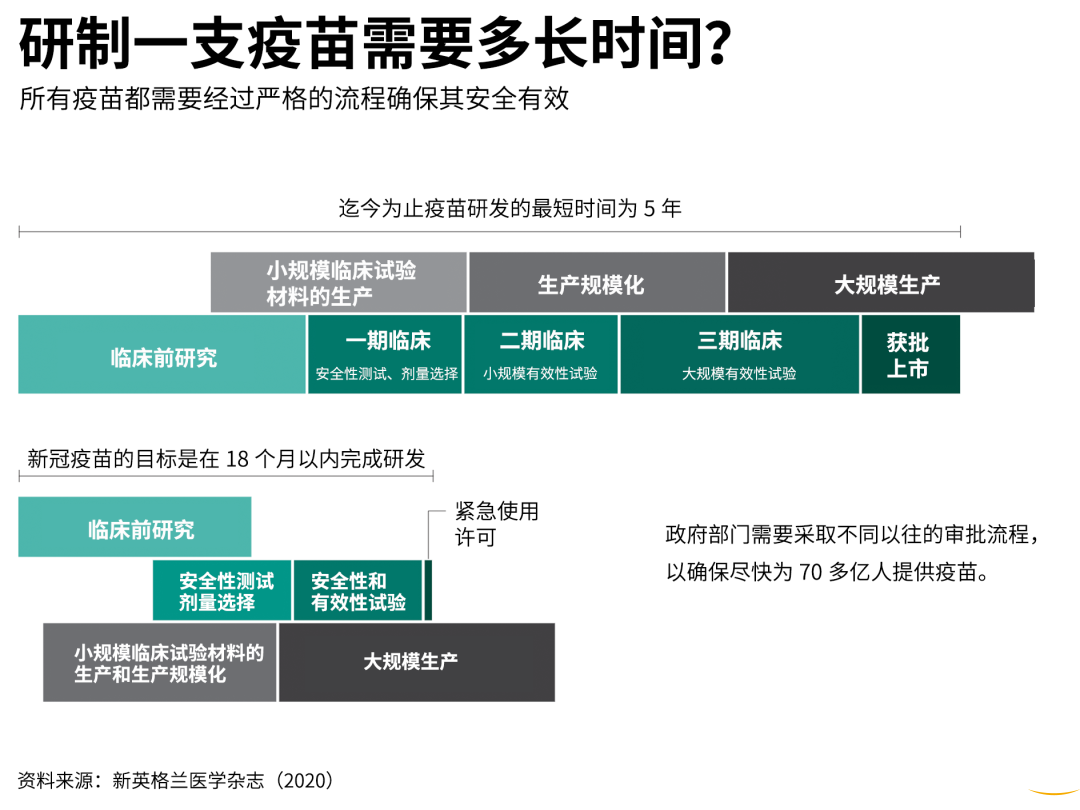
New coronavirus vaccine vs. conventional vaccine development time Source: New England Journal of Medicine
The new vaccine is expected to be available in 18 months because every step of the development process is on the "fast track”.
In preclinical sequencing, China released COVID-19 gene sequencing information within two weeks of notifying WHO of the outbreak, 10 times faster than the release of SARS sequencing results and four times faster than MERS.
On January 13, just three days after the new coronavirus sequencing results were announced, the National Institute of Allergy and Infectious Diseases (NIAID) produced a sample of the virus gene based on messenger ribonucleic acid (mRNA) technology and forwarded it to Moderna, which immediately made the first new coronavirus vaccine candidate.
In clinical trials, Moderna and Cansinotech's new coronavirus vaccine took only 66 days from the time the genetic sample was obtained to the time it entered the clinic, which is about two-thirds shorter than the 190 days for the previous "world record holder" Zika vaccine.
The WHO said at its regular briefing on new coronary pneumonia two days ago that more than 120 vaccine candidates are currently under development, and the actual number is definitely higher, some of which are undergoing clinical evaluation.
The "fast speed" is the result of technological advances and global collaboration. The new mRNA vaccine technology requires only the genetic sequencing of the virus to generate a vaccine candidate. This has greatly improved the efficiency of vaccine pre-development. However, because of the difficulty and high cost of developing the technology, no manufacturer was previously willing to invest in it.
Similarly, to support scientific research in outbreaks, WHO established the R&D Blueprint mechanism (R&D Blueprint) in 2016, which not only supports the development of clinical trial standards in outbreaks, but also includes the selection of priority directions and pathogens for R&D, the design of R&D pathways, and the proposal of product target features. With the R&D Blueprint, scientists can better target priority topics for compliant research with guidance from industry experts and all-around coordination from WHO.
Programs funded by CEPI are required to commit that the research results will benefit the entire world rather than be exclusive to individual countries, ensuring equitable access to the vaccines in future from the source of research.
CEPI has funded the development of mRNA vaccine technology over the past few years, which allowed this technology to be applied early in the current outbreak. Since the new coronavirus outbreak, CEPI has funded four projects for vaccine development, including Moderna's vaccine. As of May 11, this has expanded to nine projects and $448 million.
Can vaccines help control the outbreak?
The successful development of a safe and effective vaccine is only the first step in a long "journey to fighting the epidemic.
Once a vaccine is available, there are extremely complicate vaccine delivery issues that need to be coordinated and resolved, from production capacity to price, to access and vaccination program implementation in each country, if we want to achieve global universal immunization faster and more efficiently. So how to produce new coronavirus vaccine on a large scale and with universal access is now an issue that must be considered.
Global vaccination is a must for achieving human immunity to new coronavirus. Ideally, people in all countries will have access to the vaccine. Yet it is not difficult to imagine that whichever country takes the lead in vaccine production will be under pressure to prioritize its own needs. But if the leading vaccine-developing countries were to adopt the principle of priority given to its own people, the outcome might be disastrous for global public health.
As equitable distribution of vaccines is not just a matter of practicing humanitarianism, it is also a matter of meeting global public health needs.
No matter how much pre-preparation is done, a vaccine cannot immediately be sufficient to the globe at the beginning. If a global epidemic is to be controlled as quickly as possible, who should have priority for vaccination in the short term? This is not a question that can be solved by market bidding, but requires integrated planning and coordination among public health experts worldwide.
The question of who should be prioritized is currently inconclusive, but several groups deserve special attention. The first is the susceptible population, mainly including medical personnel, who are the closest to the virus; the second is the population prone to super-transmission events, such as employees in group accommodation, teachers, students, prisoners and practitioners exposed to large numbers of people; employees in key positions, without whom society cannot function; and the elderly over sixty-five years of age and patients with underlying diseases, who are the most vulnerable group in the face of a new coronavirus epidemic. Once infected, they will have a high risk of serious illness, complications, and death and need special protection. The prioritization of vaccination based on this principle will transcend national boundaries to minimize the death and cost caused by the new coronavirus globally and accelerate the restoration of the normal order in the society.
Globally, low-income countries are the most affected by the NICU epidemic and are "falling behind" in a dangerous way. The poorer the country, the worse the health conditions. Lack of clean water and basic medical facilities are survival challenges for the poor, and the fact that their jobs are difficult to do online makes them face loss of pay if isolated, which greatly increases their likelihood of dying from the virus.
In addition to the direct health effects of contracting the disease, poor people face worsening malnutrition, food shortages, long-term unemployment, and homelessness during the epidemic. According to UN World Food Program estimates, one billion people are already starving in low- and middle-income countries, and the number of people facing severe hunger worldwide may double by the end of the year. The United Nations Development Program even predicts that the current epidemic could reduce half of the jobs in Africa. Therefore, if low-income countries are ignored in the distribution of vaccines and the epidemic continues to spread, it will likely lead to a global humanitarian crisis with irreversible consequences.
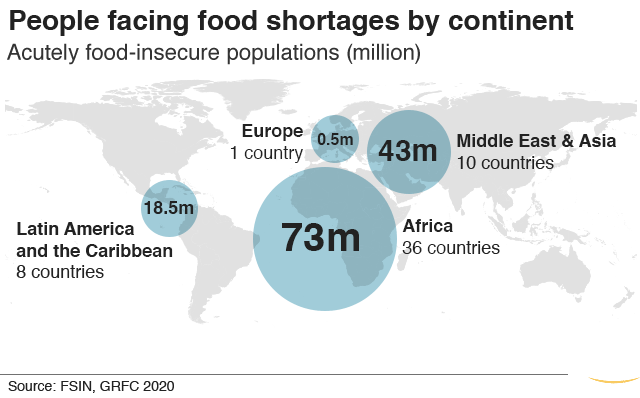
African countries face severe food shortages Photo: BBC
The 2009 influenza A (H1N1) pandemic is an example to reflect on. It took researchers only six months to make a new flu vaccine, but almost all supplies were monopolized by developed countries. Vaccine manufacturers eventually donated a small amount of vaccine to the WHO, but the amount was so small that H1N1 still caused 18,000 deaths worldwide. The new coronavirus epidemic is in many ways more frightening than H1N1 - more transmissible and deadly, with greater economic and social impact. If the history repeated itself, the world's losses would be even more devastating.
In the long term, reaching herd immunity will require universal vaccination, which means billions of doses of vaccine capacity. Building new vaccine plants often takes hundreds of millions of dollars and months, and investment in building and renovating vaccine plants needs to start now if new coronavirus vaccine is to be produced on a large scale in 12 to 18 months.
Yet this will not be easy.
Because it is not clear which technology will be tested successfully, and different vaccine technologies require different plants. Inactivated vaccines are common on the market, but not many companies worldwide are currently developing inactivated vaccines due to challenges such as the biosafety level 3 standard plants required for production. In contrast, the production of mRNA vaccines relies on the preparation of nucleic acid molecules and is advantaged in rapid and large-scale production, but due to the relatively new technology, there are not yet appropriate production facilities, technicians and quality control processes, and the need for ultra-low temperature cold chain transport, making it difficult to meet global demand. Other vaccines, such as subunit vaccines, require adjuvants to assist in improving immunity, and with limited adjuvant production, there are significant bottlenecks in vaccine production.
With an uncertain technology outlook and limited capacity for each technology line, perhaps the most prudent approach is to lay out capacity for multiple technology lines in advance. Otherwise, countries will face the embarrassment of having a vaccine successfully developed but spending months waiting for production.
Who pays for low-income countries?
Equitable access to vaccines requires large amounts of money and sufficient capacity, and these require a set of proven mechanisms to achieve them.
This brings us to the organization we mentioned earlier, the Global Alliance for Vaccine Immunization (Gavi). Gavi was established in 2000 initiated by the World Bank, WHO, UNICEF, the Gates Foundation, and national governments to procure vaccines at low cost for children in poor countries. On the one hand, by consolidating the demand from multiple poor countries, it creates a scale effect and guarantees its bargaining power with predictable and relatively large demand; on the other hand, it provides guarantees to manufacturers with long-term commitments from donor countries, thus reducing investment risks and production costs for companies and incentivizing them to continue production and R&D. In the past 20 years, Gavi has supported 496 vaccine programs in 73 of the poorest countries, vaccinating over 760 million children and reducing over 13 million child deaths.
Innovative and effective financing tools are also critical at a time when the international community needs to pull out all the efforts to curb the spreading of the epidemic.
In 2007, Gavi, with $1.5 billion in funding from the Gates Foundation and five governments, placed orders with drug companies through an Advance Market Commitment to purchase pneumonia vaccines on an ongoing basis for 73 low-income countries. Because of its good credit and large, long-term orders, Gavi has strong bargaining power when purchasing vaccines, and can often reduce vaccine prices by tens of times, making mass vaccination in poor countries economically feasible. As you can see in the chart below, Gavi can negotiate a purchase price of $27 for a vaccine worth $1,100 in the United States.
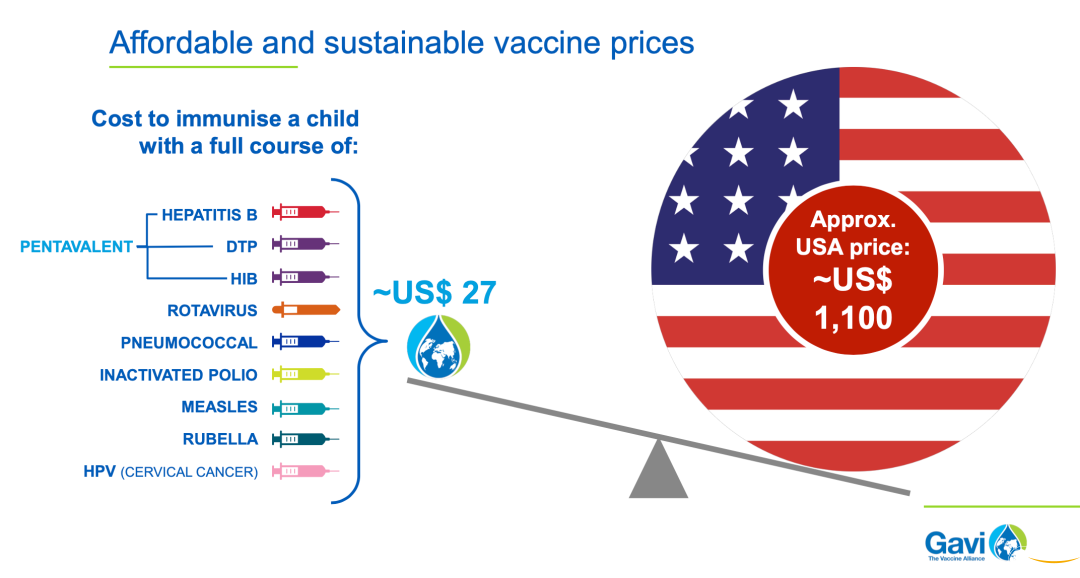
Gavi's integration of demand from poor countries has significantly reduced the purchase price.
In addition, Gavi has been financing itself in the capital markets since 2006 through "vaccine bonds". Through the International Finance Facility for Immunisation, also known as IFFIm, Gavi's vaccine bonds are borrowed in the capital markets. Gavi's vaccine debt is backed by payment commitments from governments. The competitive interest rates and the use of the product to solve a world problem have made vaccine debt a popular financial product in the capital markets.
These proven mechanisms can also be used to guarantee equitable access to the new vaccine. According to Gavi's prediction, an initial investment of $2 billion will be needed to provide vaccines to 20 million health workers, build a strategic stockpile to respond to outbreaks, and immunize high-priority groups. That's not a lot of money compared to the billions of dollars in economic losses caused by the epidemic every day.
Gavi has proposed to incentivize manufacturers to invest in large-scale production by committing to buy large quantities of vaccines at a fair price through an "advance market commitment" mechanism, while providing innovative financing, including "vaccine bonds," to expand production capacity and ensure the availability of key raw materials and equipment. Innovative financing, including "vaccine bonds," provides funds to expand production capacity, ensures the availability of key raw materials and equipment, and helps achieve technology transfer for vaccines, thereby promoting equitable access to vaccines.
Multilateral organizations and various governments have also taken actions since the outbreak, and on April 24, WHO and global partners launched The Access to COVID-19 Tools Accelerator, a global collaborative initiative to accelerate the development, production, and equitable access to new tools for the prevention and control of new coronary pneumonia.
On May 4, in response to the WHO initiative, the EU, together with interested countries, launched the International Pledging Conference for the response to the new coronary pneumonia outbreak, where countries pledged €7.4 billion and reaffirmed their internationalism by assuring low- and middle-income countries that all research results will serve the world, not limited to individual countries.
On May 19, at the World Health Assembly, the Chinese government also made five commitments, including $2 billion in international aid over the next two years, and pledged that China's new coronavirus vaccine would be developed as a global public good to ensure that the vaccine is also available and affordable to developing countries.
"Vaccine Statism" can lead to a total loss
As vaccine development progresses, "Vaccine statism" is emerging. Some countries have begun to try to obtain priority for vaccine supply from pharmaceutical companies. While governments are responsible for their own citizens, if they do not consider the global situation and allow vaccines to be concentrated in the hands of a few countries, the outcome will be a global loss. After all, as long as there are cases in any corner of the world, the international community will remain on alert and travel, production, and trade activities will not return to normal.
"Vaccine statism" is not desirable, and it shows the importance of strengthening international multilateral mechanisms. Multilateral organizations and mechanisms, including WHO, G20, CEPI, Gavi, and the Global Partnership to Accelerate the Development, Production, and Equitable Access to New Tools for Prevention and Control of New Coronary Pneumonia (GPA) initiative, have provided governments with the opportunity to discuss, coordinate, and address global issues. These organizations have accumulated the international community's valuable experience in dealing with various types of public health crises over the years and are important tools for safeguarding the common interests of humanity.
At a time when the future of vaccines is still uncertain, the supply of vaccines in all countries will face challenges. This is precisely the time when the global community is most willing to cooperate and develop equitable distribution principles, and it is a good opportunity for governments, enterprises, research institutions, the private sectors and international organizations to leverage existing systems to solve global problems.
Looking back on more than 70 years of global development since the founding of the United Nations, the international community has become an interconnected. Although the virus seems to have temporarily torn a hole in the international community, the future of humanity is interdependence, not isolation. From this perspective, the significance of the new coronavirus vaccine lies not only in saving lives, but also in restoring the global political and economic order and making up the social rift caused by the epidemic.
The Gates Foundation is 20 years old this year. The institutions and mechanisms behind the entire vaccine chain mentioned in the article can proudly say that most of them are related to the work of the foundation, and many of them were put into practice thanks to the foundation's work. There are actually a lot of breakthroughs and innovations in mechanisms, not just in technology and products. I think that's why the Foundation is focusing on these "umpopular" areas. Because first, these areas are closely connected with the well-being of humanity, and new coronavirus reminds us of this in a tragic way; second, these are the areas where innovation and collaborative thinking are needed.
I think, we should all do a better job this time.



 News
News
 Partner application
Partner application Download
Download Hot News
Hot News